Digital’s potential for improving health equity

In the post-pandemic era, the balance between those who have access to adequate healthcare and those who don’t is shifting – and health inequity is worsening. But new digital innovations are creating more opportunities than ever before to move us closer to health equity.
Health inequity has serious repercussions for a person’s length and quality of life, disability, severity of disease, and access to medical treatment. It arises due to factors outside of personal control – such as geographical location, lack of access to resources, and age, ethnic, or gender discrimination.
In the wake of the COVID-19 pandemic, health inequity is increasing in the USA as access to health insurance becomes limited to those with more stable incomes. In addition, many people don’t have the means to obtain healthcare information online. With digital content ever more prevalent in our lives, we’re learning how healthcare marketers can redress the balance to help us reach a place of better health for all.
Why is health inequity on the rise?
Health equity is widely discussed, and is a subject as concerning as it is contentious. The National Center for Chronic Disease Prevention and Health Promotion (NCCDPHP)1 defines health equity as being achieved “when every person has the opportunity to attain his or her full health potential.”
The economic downturn resulting from the COVID-19 pandemic has seen thousands of Americans lose their jobs, savings, and potentially their health cover. In 2020, the number of uninsured US citizens rose to around 31 million (8.5% of people)2 from 26 million (or 8%) the previous year3. Without proper health coverage, millions are forced to take on medical debt to cover the cost of urgent care.
Some of the significant challenges in solving, or at least improving, health equity begin by acknowledging the critical social determinants of health, power and wealth disadvantages across different sectors of society. A 2019 study published by KFF4 shows that over 80% of uninsured people are from low-income households, with adults more likely to be uninsured than children and the elderly – as are people of colour compared to white people. With the structural inequality gap widening, levels and depths of poverty have been increasing across the country.
The American Affordable Care Act (ACA) aims to make health care affordable for all, in part by supporting innovative medical care methods designed to lower the costs of healthcare5. As with every new program, there are downsides – such as the program’s inability to reach immigrants without valid documentation6 – which mean groups of people have been left ineligible for care.
Other factors contributing to the increasing divide include disparities in care (such as low-income neighbourhoods without access to hospitals and medical technology), lack of education and information, and health illiteracy. Ongoing public health and economic crises have added to educational inequality – unsuitable learning environments and a lack of resources needed to perform well mean that students from low-income families progress to lower-income jobs, perpetuating the cycle of structural inequality7. Lack of education also decreases health literacy, which is crucial for individuals to understand the health information they are given and make the best choices for their health.
Another factor in health inequity is the well-documented rise of health misinformation, particularly during the COVID-19 pandemic. Digital public health messaging will likely shape the future of healthcare in the years to come. To prevent the spread of inaccurate and potentially harmful misinformation, public health researchers have an obligation to familiarise themselves with digital strategies and collaborate with scientists, public health systems and medical experts8.
Digital public health messaging will likely shape the future of healthcare in the years to come – helping to prevent the spread of inaccurate and potentially harmful misinformation.
How did the provision of online resources change due to COVID-19?
At the start of the pandemic very few US healthcare systems had embraced virtual care at scale, with incentives to use these tools not convincing enough to overcome barriers to change. Trends like telehealth have now rapidly increased, with multiple benefits such as expanding access to care, reducing the risk of exposure to disease for staff and patients, and softening the demand on patient facilities.
Adopting changes in telehealth might continue to increase well into the post-pandemic period. For example, a recent study10 analysing COVID-19’s effects on care found that health systems are now exploring growth areas such as home health and virtual visits or service lines to support the communities they serve11. For the most vulnerable patients, access to healthcare information is vital. With the equity imbalance impacting access to technology for some sectors of society, what can we expect to see beyond the public health emergency?
Access to care online is now a basic expectation, and it provides an opportunity to evolve high-value care. While services and information are, on balance, as available today as they were before the pandemic, digital health innovation and service design improvements to enhance patient experience and health outcomes have emerged12. These could be the key to democratising and changing the way we deliver healthcare. Consider the impact of a service, such as strengthening the online visibility of hospitals. The expansion of a facility’s digital services allows organisations across the industry to reach patients quickly and easily, while implementing digital marketing techniques can build patient trust and increase the perception of reliability.
Advancements in digital have optimised healthcare resources in numerous other ways. Even at pre-pandemic levels, approximately 88% of people searched for healthcare information online, and 70% of those people made choices influenced by what they found13 – showing that digital media has the potential to become the most authoritative means for patient search.
Access to care online is now a basic expectation, and it provides an opportunity to evolve high-value care.
Could online resources and better data democratise healthcare?
The solution to democratising healthcare starts by understanding people’s health needs and concerns – and this is where data sources come in, including search volumes from search engines and social listening data insights as well as traditional sources of health data.
Weaknesses in the USA’s public health data was a critical factor in the failure of initial strategies to tackle COVID-1914. Inconsistent data reporting and gaps in testing across unequally funded communities led to a failure to spot spikes in cases and deaths. It’s become clear that improving public health data – moving away from decentralised systems and making it both equity and tech-engaged – will be integral to building a structure for housing data that counteracts inequity rather than amplifies it.
Combined with actionable information, data is the key to reaching people in a timely manner. Access to trustworthy, relevant and clear information can then empower educated decisions – and this is the role of search optimisation, accessible content and the creation of superior online experiences; demonstrating how the strength and power of data can be harnessed for good.
Powerful tools enabling patients to participate in their appointments and records are perhaps another key to digital health success15, while leveraging the omnipresence of digital applications across the country will increase coverage for those in marginalised groups.
Using data-led insights to better meet healthcare needs
While better online resources are central to improving patient access, increased data sources also benefit healthcare professionals (HCPs) and organisations within the healthcare sphere. With valuable insights into how online resources are used by HCPs, how materials are sourced and which resources are most trusted, healthcare and pharmaceutical companies can better tailor messaging to reach HCPs who would benefit most from specific resources.
Data-led analytics insights (DLA) can also help explain statistics and inform how we prioritise unmet needs in healthcare content. It is the next iteration of data-driven marketing.
In order to better understand the relationship between HCPs and online resources, we conducted a study into what over 880 HCPs think about patient resources further to the pandemic16. Our aim was to determine how and where HCPs source information and how reliable they perceive it to be, to establish if HCP needs are being met.
Insights from the Everybody research team indicate that HCPs are searching for reliable, trustworthy information in specific therapeutic areas – with 70% of respondents citing the availability of resources as either important or very important in the treatment of patients.
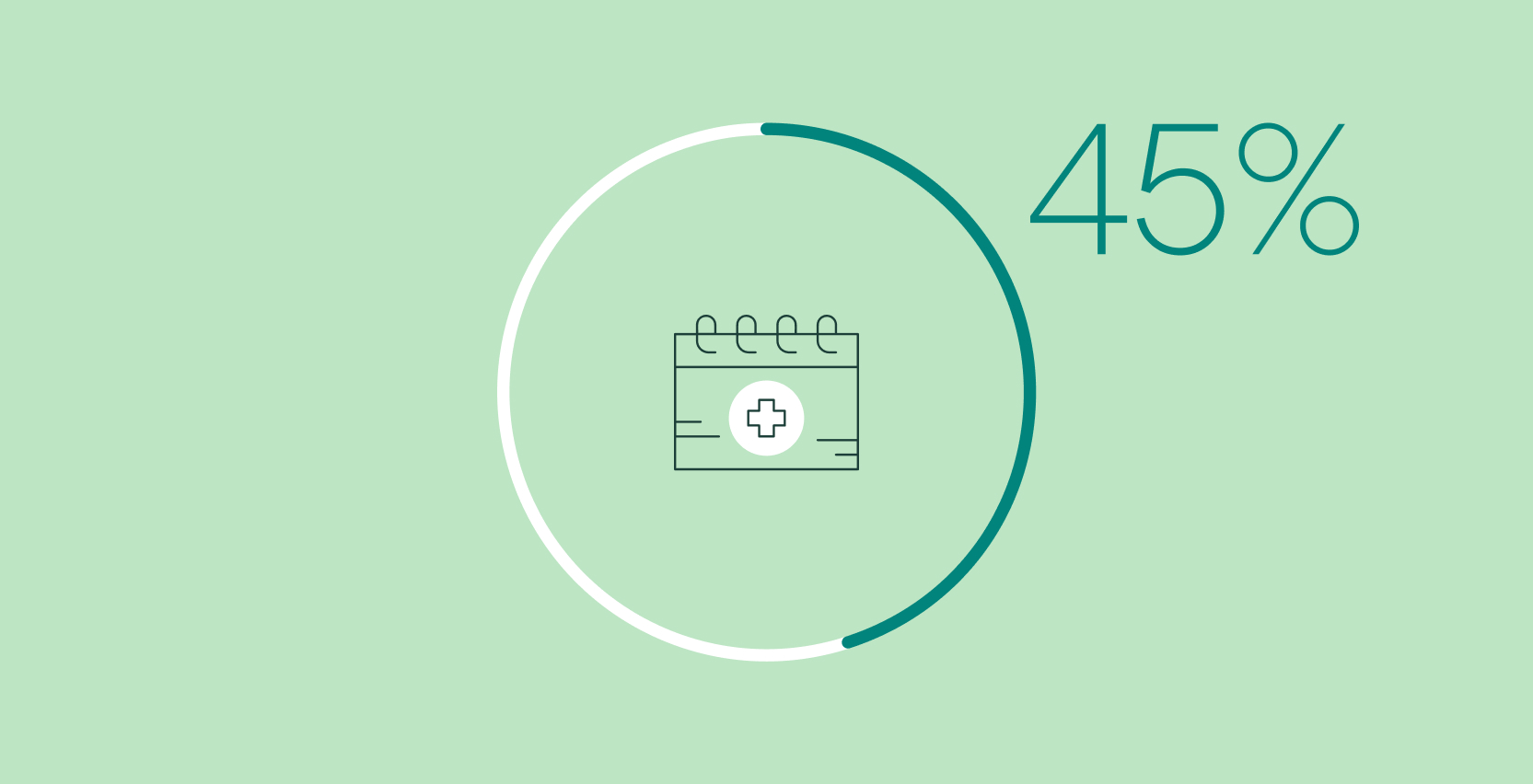
In terms of resource credibility, the data provides a similar picture, with 63% of HCPs relying on materials found through search to help inform patients about COVID-19 vaccinations. When it comes to information gathering, resources relating to treatment options, drug information and disease management are the leading search topics for HCPs, at 24%, 18% and 18% of search volume respectively.
Crucially, respondents indicate that the most valuable patient resources are those that are trustworthy, easy to use and high quality. Identifying these relevant features can help providers meet search demand by optimising content from an SEO perspective – thereby offering accurate and reliable information in critical health areas to support their patients.
With such data available across global markets, it’s clear that valuable content opportunities exist to offer patients and HCPs alike a better experience. By connecting patients with information through the creation of usable, findable content that HCPs can trust, pharmaceutical companies and other health care providers have the power to improve patient outcomes. For example, frequent updates to monitor and maintain quality content can enhance the relevance and integrity of searchable sources, while access to appropriate resources can improve health literacy and empower patients to make good health care choices.
Insights from the Everybody research team indicate that HCPs are searching for reliable, trustworthy information in specific therapeutic areas.
How can marketers help pharmaceutical companies and HCPs initiate change?
The provision of content and access to healthcare professionals online is part of digitising healthcare for low-income families and those defined by geographical limitations. From connecting families in poorer areas and those without the means to travel, to diversifying the data available for analysis, marketers can help healthcare organisations improve the provision of online resources.
A functioning digitised health system can revolutionise how the industry relates to patients. Recognition of disease, smarter supply chain systems and better efficiency are all benefits of improved digitisation. With the population living longer and low and middle-income families struggling to pay for healthcare, digital systems can identify opportunities to implement solutions for the prevention, treatment and monitoring of population health17. Of course, these improvements will concurrently mean a focus on data ownership and ethical considerations, such as privacy policies, to ensure the protection of the rights of individuals.
The digital road to health equity
Understanding patient needs is the key to improving therapy insights and, ultimately, bettering patient health18. For healthcare companies who want to be part of the solution, focusing on patient resources that improve health literacy and providing better digital healthcare options will be crucial in helping us move closer to health equity.
Marketers have a significant role to play in ensuring healthcare companies provide improved access to resources. Healthcare services and organisations need the right solutions to reach patients – and developing rich, relevant, impactful research and strategies can positively shape communications between HCPs and healthcare consumers, while digital data can help HCPs make decisions regarding future development and help organisations effectively deliver services.
By providing healthcare professionals with trustworthy and relevant information, along with the tools to use it, marketers can help HCPs better meet the specific needs of their patients19 and offer improved and more equitable digital experiences for all.
Everybody has produced this article as part of our ongoing commitment to producing quality healthcare content with a global focus.
We're committed to working with our client partners to improve health equity
Contact us to learn more about what we're doing and how we can work together.